Cornea Cross Linking Procedure
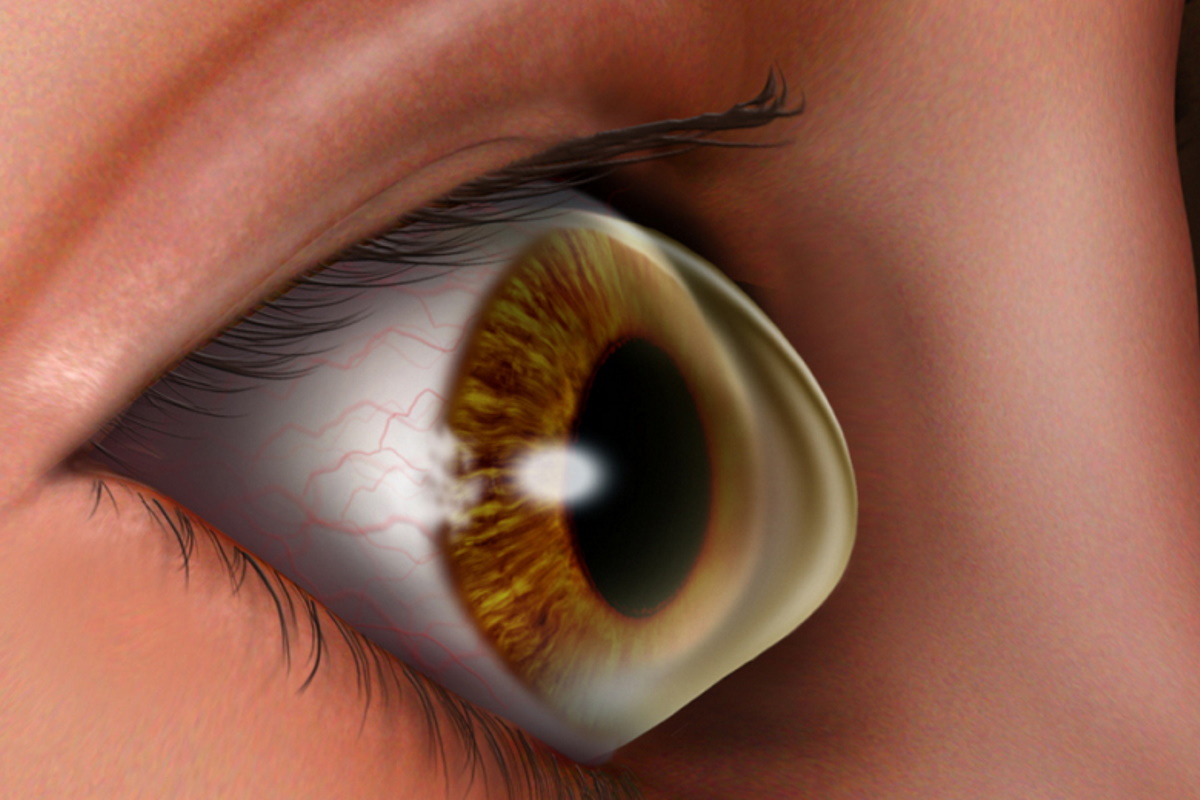
Keratoconus is a condition where your cornea becomes thinner and changes shape from being a regular round to an irregular cone or oval shape resulting in blurred vision. In the past, corneal transplant was the only treatment option but since 2016, corneal cross linking (CXL) was FDA approved to treat and prevent progression of keratoconus.
CXL involves applying liquid riboflavin (Vitamin B2) to the cornea and exposing it to ultraviolet light. The cross linking process stiffens the cornea’s structure and may slow and even stop the progression of keratoconus. It is believed that the cornea becomes strengthened and ultimately, may prevent the necessity for corneal transplants for these keratoconus patients. It is very important to understand that CXR therapy is to prevent the cornea from getting worse and NOT to improve the vision. With this therapy, many patients with keratoconus or other corneal ectatic (thinning) disorders may be able to avoid the need for corneal transplantation.
Click to view Moorfields Eye Hospital video on Cornea Cross Linking
Treatment Process
- Your eye will be numbed using anaesthetic eye drops
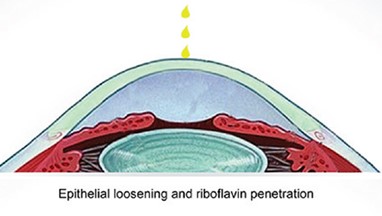
- A layer of your corneal epithelium will be removed
- Riboflavin eye drops are applied on the corneal surface and allowed to soak into the cornea
- Ultraviolet light is shone on to the eye to start the process of cross lining between the Riboflavin and the collagen molecules in the cornea
- A soft contact lens is applied on your eye at the end of the procedure and will be removed by your eye doctor at the next clinic visit
Post-op Care
- There will be eye discomfort for the first 2-3 days while the cornea heals. You will be provided with eyedrops to keep the eye comfortable and also to prevent any eye infection. Sometimes, you may need to take some oral pain medication
- You will be sensitive to light and as such, wear sunglasses to reduce the glare
- Try to have more rest during the healing period and reduce any activities causing eye strain like reading, looking at the computer or playing games on your mobile phone
- It is quite normal for the vision to get a bit worse for the first few weeks after the treatment


Follow up
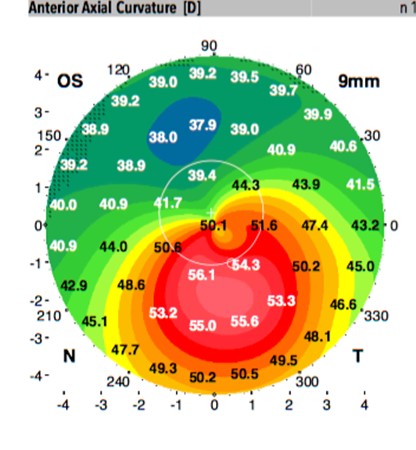
Have regular follow-up eye examinations with your eye doctor to monitor the progression of the keratoconus. It is important to detect any deterioration early and have treatment quickly so that the keratoconus does NOT progress to cause irreversible scarring.
Discuss your Treatment Options for your corneal condition with a Corneal Eye Specialist
Disclaimer. TELEME blog posts contains general information about health conditions and treatments. It is not intended to be a substitute for professional medical advice, diagnosis or treatment. The information is not advice and should not be treated as such.
If you think you may be suffering from any medical condition, you should seek immediate medical attention from your doctor or other professional healthcare providers. You should never delay seeking medical advice, disregard medical advice, or discontinue medical treatment because of information on this website.