Post-Operative Care after Brain Surgery
Craniotomy (also known as open brain surgery) is the first line treatment for brain tumours which are large or accessible near the skull surface. The goal is for the surgeon to remove all (or as much as possible) of the brain tumour and to provide relief from the pressure effect that the tumour is causing to the normal parts of the brain. Successful surgery will bring relief to the symptoms of headache, nausea or vomiting, loss of balance, weakness etc which the brain tumour may be causing.
Risks of Brain Surgery
Brain surgery, like any surgical procedure, carries risks. However, advances in surgical techniques and technology have significantly reduced these risks. These risks include;
- Swelling (oedema) of the brain is common and may cause temporary neurological symptoms. Steroid medications are often used after surgery to reduce the swelling and minimise these effects
- Bleeding (Haemorrhage) can occur during or after surgery. While significant bleeding is uncommon, it may require additional treatment, such as a blood transfusion or further surgery to stop the bleeding
- Infection may occur (as with any form of surgery). Antibiotics are often administered before and after surgery to minimise this risk
- Seizures may occur after brain surgery. Anti-seizure medications are often prescribed to prevent this
- Neurological Deficit (whether new or pre-existing) occurs depending on the tumour’s location. Surgery may cause temporary or some permanent neurological deficits (such as weakness, numbness, or speech difficulties)
Recovery Process
Recovery from brain tumour surgery varies depending on the individual patient, the type and location of the tumour, and the extent of the surgery. The recovery process typically involves a combination of medical care, rehabilitation, and follow-up appointments.
1. Hospital Stay
After brain surgery, patients are usually monitored in the intensive care unit (ICU) for the first few days for close observation. During this time, the healthcare team closely monitors the patient’s neurological function, vital signs, and overall condition. Most patients can expect to stay in the hospital for about five to seven days, depending on their recovery progress.
2. Physical Rehabilitation
Rehabilitation is a crucial component of the recovery process. Depending on the tumour’s location and the surgery’s impact, patients may require physical, occupational, or speech therapy to regain strength, mobility, and cognitive function.
- Physical Therapy focuses on improving strength, balance, and coordination. It is especially important for patients who have experienced weakness or paralysis before (or as a result of) the tumour or surgery to be assessed and treated by a physiotherapy team
- Occupational Therapy helps patients regain the ability to perform daily activities, such as dressing, eating, and bathing. It also addresses any challenges related to fine motor skills, such as writing or buttoning clothes
- Speech Therapy may be necessary for patients who experience speech or language difficulties after surgery. Therapy sessions focus on improving communication skills, such as articulation, fluency, and comprehension
3. Cognitive Rehabilitation
Cognitive rehabilitation is designed to help patients regain cognitive functions that may have been affected by the tumour or surgery. This type of therapy focuses on memory, attention, problem-solving, and executive function.
- Memory Exercises: Therapists will work with patients on exercises and strategies to improve memory, such as using mnemonic devices, creating routines, and keeping a diary
- Attention Training: Patients may undergo exercises to improve their ability to focus and maintain attention on tasks
- Problem-Solving Skills: Cognitive rehabilitation may also involve exercises to enhance problem-solving and decision-making abilities, helping patients return to daily life and work
Follow-Up Care
Follow-up care is essential for monitoring the patient’s recovery and detecting any signs of tumour recurrence. Patients typically have regular follow-up appointments with their neurosurgeon and oncologist to review brain scans (MRI or PET scans), assess neurological function, and adjust the treatment plans as needed.
- Medication Management: Patients may be prescribed medications to manage symptoms, such as anti-seizure drugs, steroids to reduce swelling, or pain relievers. The healthcare team will adjust medication dosages based on the patient’s progress.
- Lifestyle Adjustments: Patients may need to make lifestyle adjustments to support their recovery and overall health. This can include adopting a healthy diet, staying physically active, avoiding alcohol and tobacco, and managing stress or depression
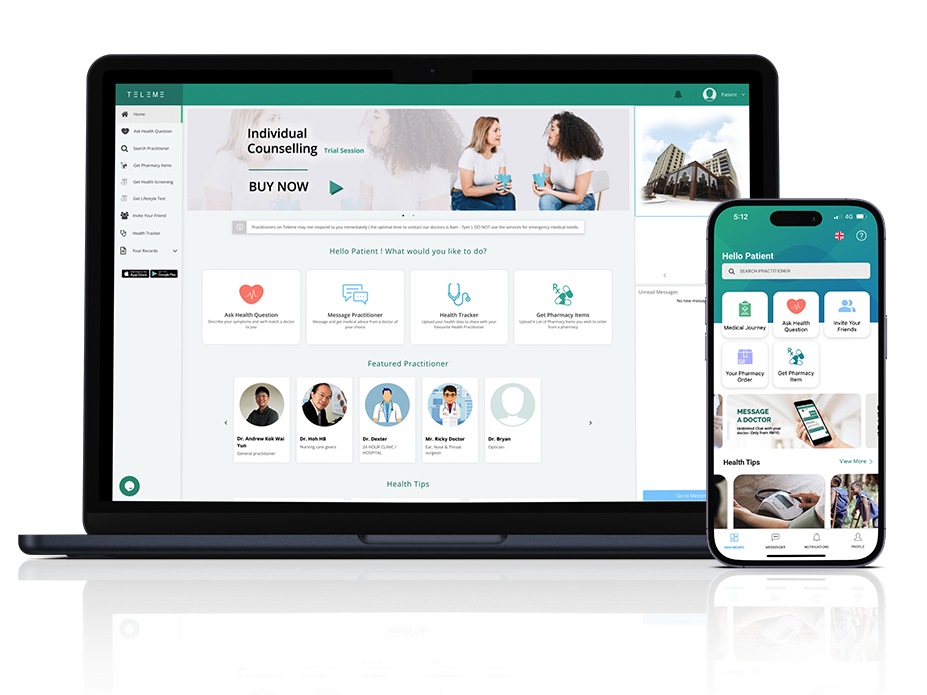
Discuss your Treatment Journey with your Brain Surgeon, Oncologist, Physiotherapist, Occupational Therapists and Speech Therapist
Disclaimer. TELEME blog posts contains general information about health conditions and treatments. It is not intended to be a substitute for professional medical advice, diagnosis or treatment. The information is not advice and should not be treated as such.
If you think you may be suffering from any medical condition, you should seek immediate medical attention from your doctor or other professional healthcare providers. You should never delay seeking medical advice, disregard medical advice, or discontinue medical treatment because of information on this website.